This Week in Mac Sports: 9/15
Malaria Treatment
Malaria can be a potentially fatal disease especially when caused by Plasmodium falciparum. Treatment should be initiated as soon as possible after diagnosis is made. Treatment can be both by oral drugs as well as intravenous injections of antimalarials. Most drugs used in treatment are active against the parasite forms in the blood.
Choice of treatmentTreatment of a malaria patient depends on several factors including;
Treatment promptly with antimalarial agents can usually result in a full recovery. Drugs that are used to prevent malaria in travellers are also useful in treatment of malaria. Sometimes a combination of different antimalarials may be prescribed to overcome strains of malaria that have become resistant to single types of medication.
Antimalarial medication is usually given as tablets or capsules. Hospital admission is needed for severely ill patients, patients with Plasmodium falciparum malaria, mixed infections and unidentified strains of malaria. There are several types of antimalarials used to prevent and treat malaria.
Drugs used in treatment of malaria include:-
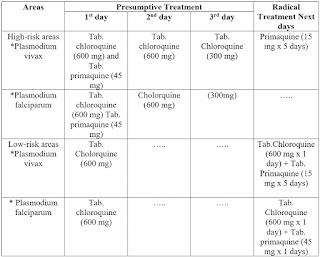
These patients are usually not admitted to the hospital for treatment and can be treated in the out-patient department unless there are complications. Chloroquine as the drug of choice for the treatment of all non-falciparum malaria. It is highly effective against P. Malariae and Plasmodium ovale and most strains of Plasmodium vivax.
There are areas with strains resistant to choloriquine. Malaria from and in these areas can be managed by other agents like quinine, artemether with lumefantrine or atovaquone-proguanil.
Before prevention of relapse primaquine is used. It destroys the liver stage parasites. For treatment of P. Ovale 15 mg primaquine/day for 14 days and for some strains of P. Vivax higher doses of primaquine - 30 mg primaquine/day for 14 days may be used. G6PD activity should be measured in Plasmodium vivax or Plasmodium ovale infections as the primaquine can cause haemolysis (break down of RBCs) in those with G6PD deficiency.
Recommendations for patients with falciparum malariaAs per recommendations, all patients with falciparum malaria should be admitted to hospital initially. These patients need supportive management in the HDU (highly dependent unit) or ICU in presence of complications.
Treatment is usually with oral quinine sulphate 600 mg every 8 hours for 5-7 days plus doxycycline 200 mg daily (or clindamycin 450 mg every eight hours for pregnant women) for 7 days.
Another alternative is Atovaquone-proguanil 4 standard tablets daily for 3 days. Treatment is also effective with Artemether with lumefantrine (Riamet®). The dose for patients over 35 kg is 4 tablets at once and then a further 4 tablets at 8, 24, 36, 48 and 60 hours.
Recommendations for patients with severe or complicated falciparum malariaThese patients require intravenous drugs. Intravenous quinine dihydrochloride is usually the first line agent. Initial dose is 20 mg/kg (to a maximum of 1.4 g) over 4 hours, followed by 10 mg/kg (to a maximum of 700 mg) every 8 hours for the first 48 hours or until the patient can swallow. Once the patient can take oral drugs quinine sulphate 600 mg thrice a day is given to complete a 5-7-day course in total.
The artesunate regimen is usually given as an IV injection, repeated at 12 and 24 hours and daily thereafter. Intravenous artesunate has not been licensed in the European Union but there is accumulating evidence that it offers a significant benefit over quinine where patients have very severe malaria or high parasite counts.
Alternatively a second drug can be given with these regimes. These include doxycycline 200 mg once daily or clindamycin 450 mg thrice daily (for pregnant women) for a total of 7 days from when the patient can swallow.
Further ReadingWhat Is Malaria?
Malaria is a serious and sometimes deadly infectious disease caused by a parasite and spread through mosquito bites. The disease is a public health concern worldwide. In fact, an estimated 247 million people contracted malaria in 2021 alone—causing more than 600,000 deaths as a result of the disease.
The mosquitoes that carry malaria are usually found in tropical environments around the equator. This includes places such as Central America, sub-Saharan Africa, and parts of Asia. However, the U.S. Reports nearly 2,000 cases of malaria each year, mostly due to travel to tropical places.
Most people who develop malaria experience high fever and other flu-like symptoms. It's important to treat symptoms as quickly as possible, as the condition can rapidly become severe and cause life-threatening complications.
Symptoms of malaria can range from mild to severe. Most people experience symptoms between 10 and 15 days after they've been exposed to the disease. If you have malaria, it's common to experience flu-like symptoms including: However, if your condition worsens, you might experience severe malaria symptoms such as: Extreme fatigue Convulsions or seizures Loss of consciousness Difficulty breathing Abnormal bleeding Dark or bloody urine Jaundice (yellowed eyes and skin) The World Health Organization recommends receiving prompt medical care by visiting your local emergency department or calling 911 if you experience severe symptoms. Most people who have malaria get bit by a mosquito who was carrying the disease. Malaria is caused by a tiny parasite (or, a harmful organism that feeds on a larger organism). In this case, the larger organism is a mosquito. The mosquito can then pass the disease to you if it bites you and the parasite infects your blood cells. Malaria can affect anyone, but it's most common among people living in tropical environments where malaria is easily spread. The following groups may also be at a higher risk of developing severe malaria symptoms: Young children Pregnant people People living with HIV/AIDS People in areas with limited access to healthcare or medical resources If you think you may have been exposed to malaria or are experiencing symptoms, it's essential to seek medical care as soon as possible. This is so that the disease doesn't progress and causes life-threatening complications. During a visit with your healthcare provider, you can expect them to ask about your medical history and recent travels, conduct a physical exam, and order routine blood tests to identify the severity of your condition. Your provider may also order malaria-specific tests, including: Microscopic diagnosis: Uses a sample of your blood and inspects the sample under a microscope to check for parasites. This exam is considered the gold standard for malaria testing. Rapid diagnostic tests (RDTs): You will place a sample of your blood on a test card and receive the results within 15 minutes. Providers use this test in settings where laboratory testing or access to microscopes aren't readily available. It's important to note that in the U.S., a malaria diagnosis is not common. In fact, healthcare providers and laboratory technicians alike tend to not have a high suspicion for malaria since the condition is rare in the country. If you have symptoms of malaria—especially after traveling to a location where the disease is more common—there may be a delay in getting your diagnosis and treatment. That said, as soon as you notice you have symptoms of malaria or are feeling unwell, it's important to see your healthcare provider so they can get you tested as soon as possible. The standard treatment for malaria is medication. Your healthcare provider may choose one or a combination of medications to help you reduce symptoms. Most medications come in pill form, but some people may receive injection medications from their provider's office or hospital. The most common medications to treat malaria include: Coartem (artemether-lumefantrine) Aralen (chloroquine) Jasoprim (primaquine) There are several prevention strategies that you may consider using to avoid contracting malaria. These may be especially important to use before you visit areas where malaria is more common. You may consider trying the following methods: Getting your child vaccinated with Mosquirix (the RSS,S/ASO1 vaccine for malaria) Limiting your risk of attracting mosquitoes by using mosquito nets while sleeping, putting mosquito repellent on your belongings and clothes, wearing clothing that covers your arms and legs, and avoiding keeping windows and doors open Talking to your healthcare provider about antimalarial medications before and after traveling, which can prevent you from getting sick if you do get mosquito bites during your trip It is imperative to treat malaria quickly to prevent life-threatening complications from occurring. The more severe your condition gets, the higher your risk of experiencing organ failures and changes to your blood supply. If the condition is left untreated or treated too late, you may experience: Many of these complications can also be fatal (deadly), which is why getting medical care as soon as you may have been exposed to the disease is essential. Malaria is a serious, but treatable condition that is caused by parasites and transmitted through mosquito bites. The disease remains one of the most common public health problems worldwide. While malaria is less common in the U.S., you may contract the condition if you travel to tropical environments where the disease is more common. If you develop symptoms of malaria or feel sick after you return from your travels, it's good practice to see your healthcare provider for care. They can learn more about your symptoms, order tests that offer a proper diagnosis, and get you started on treatments. If malaria is left untreated, you may be at risk of developing life-threatening complications. That's why receiving the proper care as soon as possible is important.Novel Noninvasive Test For Malaria Does Not Require A Blood Sample
A novel testing platform under development by researchers at the Yale School of Public Health (YSPH) and CytoAstra, LLC could provide a new noninvasive test for malaria that doesn't require a blood sample.
The platform technology, known as cytophone, detects malaria infection in blood cells using lasers and ultrasound. Researchers developing the platform believe it could provide more sensitive and reliable testing results compared to the more traditional blood tests for malaria, which require a blood sample and tend to detect malaria only at higher parasite burdens, hindering effective detection and treatment.
The research team recently received a $500,000 grant from the Bill & Melinda Gates Foundation that will allow them to build two improved prototypes of the testing platform and to do extensive field testing in Burkina Faso, where malaria is endemic, said Dr. Sunil Parikh, an associate professor of epidemiology (microbial diseases) at YSPH and of infectious diseases at the Yale School of Medicine. Parikh is a co-principal investigator on the project.
Malaria is an enormous health problem globally. In 2021 (the most recent year for which data is available), nearly half of the world's population lived in an area where malaria is endemic, according to the World Health Organization (WHO). There were an estimated 247 million malaria cases that year — an increase of 2 million compared with 2020 — and 619,000 deaths, according to the WHO. Young children, pregnant women, and nonimmune travelers are the most vulnerable to severe infection.
Parikh's co-principal investigator is Vladimir Zharov, director of the Arkansas Nanomedicine Center at the University of Arkansas for Medical Sciences and co-founder of CytoAstra, a company advancing cytophone research. CytoAstra is a sub-award recipient of the foundation grant. Zharov, a pioneer in noninvasive technologies for medical applications, has previously applied cytophone technology for the noninvasive detection ofcirculating melanoma cells. Realizing the platform's potential application for human malaria, Zharov teamed up with Parikh, whose research centers on malaria interventions in Africa, to develop a portable cytophone prototype that could detect malaria infection in people living in endemic settings.
For malaria, the cytophone technology uses lasers at specific wavelengths focused on superficial blood vessels. When the parasites that cause malariainfection enter red blood cells, they use the hemoglobin inside those cells to liberate amino acids.
A byproduct of this process is the release of hemozoin, a compound containing iron. When hit by a laser, hemozoin absorbs more of the laser's energy than hemoglobin, meaning cells infected with malaria parasites absorb more than noninfected cells. This absorbed energy is transformed into heat, and the heat expansion generates acoustic waves. The cytophone technology detects these waves using a small ultrasound transducer placed on the skin. After software analysis, peaks in the detected acoustic waves can identify malariainfection.
In a prior study published in Scientific Reports, Zharov and Parikh showed their device could identify infection in mice using a rodent species of malaria parasite and in blood using a human malaria parasite.
The Zharov team then developed a portable version of the device and the researchers jointly completed a human proof-of-concept study in malaria-infected adults in Cameroon with Professor Yap Boum, currently executive director of the Pasteur Institute of Bangui, and a long-standing collaborator of the Parikh lab. The results were promising and are under review for journal publication, Parikh said.
Parikh praised the multidisciplinary collaborative effort with Zharov and their Cameroonian colleagues in advancing the technology. Working together "opened doors that we would never have been able to open separately," he said.
The cytophone technology could represent a big improvement in diagnosing, treating, and understanding malaria, said Parikh.
Malaria is currently diagnosed by two methods. In light microscopy, long the standard for diagnosis, blood is smeared on a slide, stained, and studied under a microscope. But because this requires resources and expertise, it is being replaced in many areas by rapid antigen blood tests. These are designed to react to the presence of a specific antigen, or protein found on the surface of a pathogen, in a sample.
A problem with both methods is that they aren't very sensitive.
You can have a very large parasite load with both microscopy and rapid diagnostic tests before you have a positive test."
Dr Sunil Parikh, Associate Professor of Epidemiology and Infectious Disease, School of Medicine, Yale University
Because the cytophone technology can potentially scan a much larger volume of blood, it should be far more sensitive than current tests, Parikh said. The technology also could address an emerging problem with some antigen tests, he added.
In Africa, the most common antigen tests search for an antigen on Plasmodium falciparum, the locally dominant of the five species of protozoa that cause human malaria, and the most dangerous. But researchers are finding more and more samples of the parasite with deletions of that antigen. In some places, most of the parasites no longer express that antigen, Parikh said.
Since cytophone uses hemozoin, which all species of malaria parasites produce as part of their life cycle, as a marker, it would avoid this problem, Parikh said.
"We don't think that there's ever a situation where hemozoin wouldn't be present over the life cycle of the parasite," he said.
In addition to diagnosis problems, a challenge plaguing malaria treatment in the long term is that the parasites become resistant to medications. Since the technology focuses on hemozoin, it could be useful to researchers trying to develop and study new antimalarial drugs that target this pathway in humans, noninvasively, Parikh said. "I think that would be a really exciting avenue for this device."


Comments
Post a Comment