Tuberculosis Is the Oldest Pandemic, and Poverty Makes It Continue - Scientific American

Meera Yadav gave birth to her first baby in 2013, when she was a 23-year-old living in a slum in Mumbai, India, with her husband's family. She was filled with joy and hopes for a bright future. But four months later she began having fevers and coughing up blood.
Yadav's husband took her to a private hospital, where a doctor prescribed blood tests, a chest x-ray and a sputum test.
She was diagnosed with tuberculosis, a disease at least 9,000 years old that has likely killed more people than any other plague—as many as one billion in the past 200 years. Although the illness may seem like a historical footnote in high-income countries, it continues devastating poorer nations, afflicting the most disadvantaged: poor people, prisoners and those who are HIV-positive.
TB is a bacterial infection caused by Mycobacterium tuberculosis. It spreads when someone coughs, pushing bacteria into the air. In most cases, the immune system stops the bacteria from growing. It can remain in the body, dormant but alive, for years without causing symptoms or spreading. These cases are difficult to detect because people have normal chest x-rays and negative sputum tests.
But for about 10 percent of infected people, like Yadav, the infection develops into a serious disease and becomes contagious. Nearly two billion people—one quarter of the world's population—are infected today. Roughly 10 million fall ill annually. Without treatment, most cases lead to prolonged illness that culminates in fatal respiratory failure; TB kills about 1.5 million people every year.
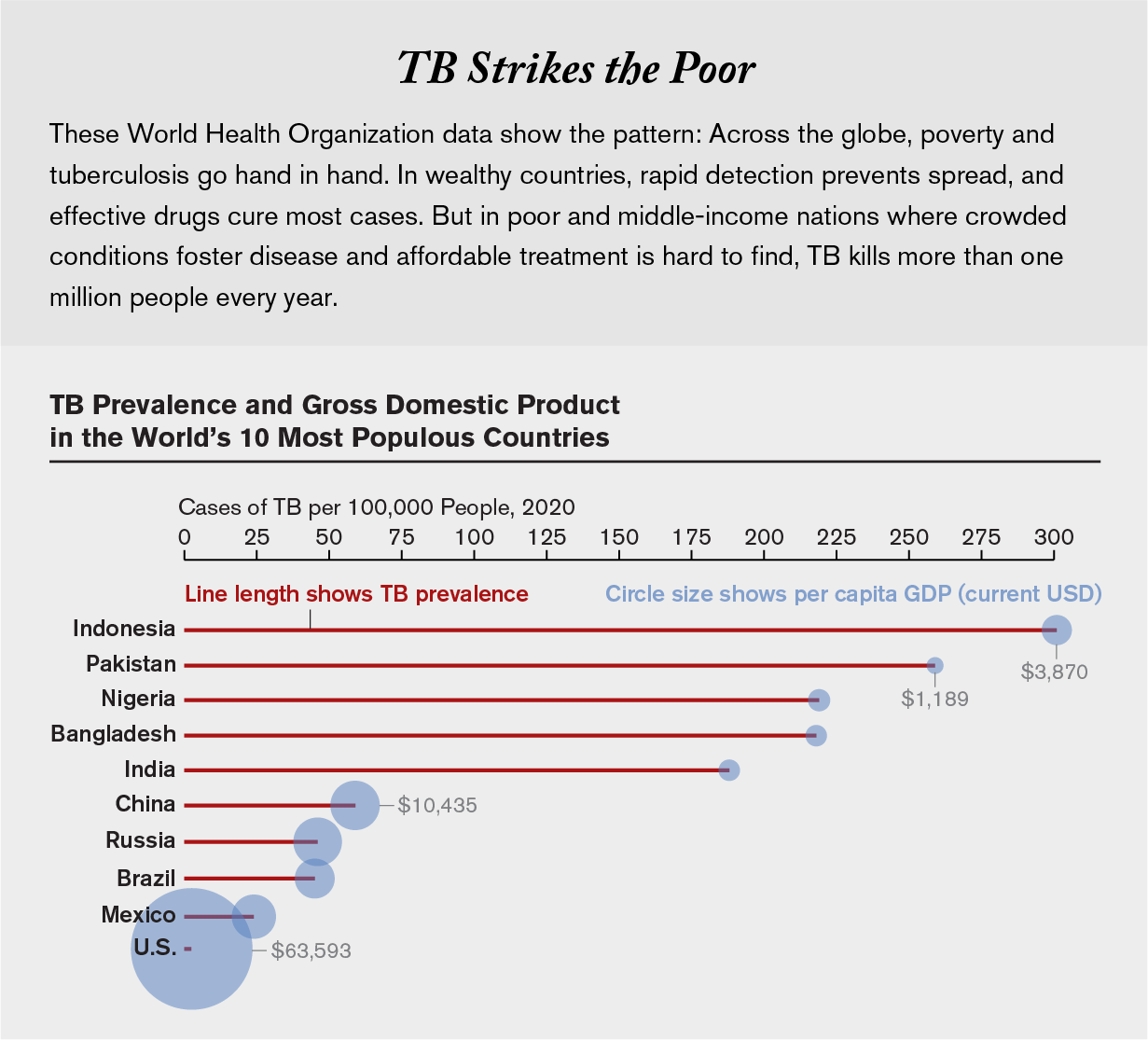
The World Health Organization estimates that more than 95 percent of these deaths are in low- and middle-income countries where malnutrition, lack of health care and crowded housing allow the disease to thrive and spread. In these places, inadequate public health systems fail to detect many cases, and effective treatment may be too expensive or unavailable. "Wherever there is poverty within a country, TB will find such people," says epidemiologist Madhukar Pai, a TB expert at McGill University. "It's mostly Black, brown, Indigenous and poor people who suffer from TB, and that's why it doesn't get much attention."
It was easy for TB to find Yadav. She was living in poverty amid dilapidated houses stacked close together. Mumbai is one of the worst hotspots in India, a nation that accounts for one quarter of all diagnoses worldwide.
There is a desperate need for more research on TB. The one existing vaccine is ineffective in adults and almost a century old. Many strains of TB have developed resistance to antibiotics, and some are resistant to many or all drugs used to treat the disease. For years the WHO has been calling on nations to invest in developing better drugs and diagnostics. The agency estimates that an extra $1.1 billion is needed every year.
In recent years, global TB cases declined about 2 percent annually, too slow to hit the United Nations goal, announced in 2015, of ending the pandemic by 2030. The COVID pandemic exacerbated TB, overwhelming national health systems, making it impossible for many patients to receive treatment and pushing more people into poverty. "Even before the pandemic, we were not making good progress," Pai says. "But the past two years have been so bad that we have lost something like 10 years of progress in TB." In 2021, for the first time in more than a decade, TB mortality increased.
Despite this slide, there are reasons for hope. Across the globe, innovative initiatives focused on the most vulnerable patients are targeting prevention, detection and treatment. None of these efforts alone will vanquish TB. But they point the way forward to a future in which the disease is no longer neglected.
Fighting the Resistance
After her diagnosis, Yadav was hospitalized for a month, at a cost of 300,000 rupees (almost $4,000), arduously paid by her husband's family. Once home, she was separated from her newborn, and her relationship with her husband and in-laws soured. "They all discriminated against me because I had TB," she remembers. Despite treatment, she did not improve.
Her husband took her to a second hospital, where they diagnosed her with MDR-TB (multidrug-resistant tuberculosis). Her treatment now involved 13 different medications, including injections of kanamycin, which can cause permanent hearing loss and kidney impairment. Instead of the six-month course that cures most TB, MDR-TB treatment can last as long as 48 months, with a success rate of only 59 percent. India estimates that about 130,000 people get sick with MDR-TB every year, but less than half of those cases are diagnosed, and even fewer are treated. Errors in diagnosis and treatment fuel the transmission of drug-resistant TB.
"We [doctors] are somewhat responsible for the increase of MDR-TB," says pulmonologist Vikas Oswal, who divides his time as a TB physician between public and private sectors in Mumbai. Medical errors and failure to follow up on patients are common, especially in the private system. In India, public-sector TB treatment is free, but patients often face long lines. Instead more than half seek private care, which is faster but not as prepared to deal with TB. Most private clinics don't have access to medications to treat MDR-TB, and doctors see as many as 14 patients at the same time in an exam room, he says.
Seven months after her second round of treatment, Yadav's fever came back, and she woke up early one morning coughing blood. A CT scan showed her right lung was collapsing and had to be removed. She spent another month in the hospital, at which point her husband's family evicted her and took custody of her son. She moved back to her parents' house, where her mother was already suffering from a case of untreated TB that would soon kill her. "I attempted suicide twice," Yadav says. "I asked myself: Why me? I questioned why God had chosen me to bear all that."
Three years after her initial diagnosis, a friend referred Yadav to a Doctors without Borders clinic in Mumbai. They offered to treat her for free, this time with newer drugs. With help from psychologists, she convinced herself to try again, mostly for the sake of her son. She got bedaquiline and delamanid, two potent and less toxic medicines for MDR-TB introduced in 2012. "These drugs saved my life," Yadav says. In 2018, almost six years after her diagnosis, she was cured. The WHO now recommends both drugs as standard treatment for MDR-TB, but access is an issue in India.
Until 2019, the country relied on pharmaceutical company donations of these medicines. Today the government pays about $350 for a six-month course of bedaquiline and $1,200 for delamanid. The prices are too high for India to treat all who need it. In 2019 alone, 66,255 people were diagnosed with MDR-TB in India, but only 2.6 percent received the newer drugs.
In 2021 Yadav and another TB survivor filed a petition in the Bombay High Court requesting the national government invalidate the medications' patents—which expire after 2023—allowing Indian drug companies to manufacture cheaper generic versions. The lawsuit, delayed because of COVID, is unlikely to succeed: India has issued this kind of license only once before, for a cancer drug in 2012.
Yadav remains hopeful about the case. She still gets breathless quickly and must regularly drain liquid from her lung. But she has found inspiration in fighting for other patients. "I want to make sure that no one has to suffer what I did," she says.
Dangerous Air
Children are especially vulnerable to developing severe TB; they account for 11 percent of cases and 13.8 percent of deaths worldwide. But prevention and treatment usually focus on adults, who are more likely to spread the disease, and children are often overlooked. Of the estimated 200,000 children who die of TB every year, 90 percent are never diagnosed or treated.
A South African program, led by national and municipal departments of health in partnership with Doctors without Borders, protects members of this vulnerable group living in the shantytowns of Khayelitsha and Eshowe.
Nurse Ivy Apolisi wanders the unpaved alleys of Khayelitsha, searching for her patients among tiny shacks made of tin, wood and cardboard. Here most homes lack formal addresses, indoor toilets, running water or electricity. Families of 11 or more often share a single room with little or no ventilation. "If one is coughing, it is so easy to infect another," she says. Khayelitsha has one of the highest burdens of TB in the country, with surging cases of drug-resistant strains.
Apolisi, together with a physician colleague, ensures that children in close contact with her TB patients take the daily preventive medication isoniazid for at least six months, as recommended by the WHO. The practice is routine in wealthy nations but not poorer ones.
In Khayelitsha, COVID brought a spike in TB transmission and mortality. Children stayed indoors, sharing air with their sick relatives. So the team began making house calls rather than asking adults diagnosed with TB to bring their children to clinics. Apolisi checks any children in the household for signs of TB. Children with symptoms head to the clinic for tests. Those who are not ill get preventive treatment. Some are as young as six weeks old. For children up to three years old who can eat solid food, the team dissolves the medicine in mango yogurt, an exciting treat for them. "Preventing TB in children is much better than watching and waiting to see if they will get sick," Apolisi says.
Only 2.8 million people worldwide received preventive medication in 2020, a 21 percent slide from 2019. "We are not doing nearly enough to prevent TB and drug-resistant TB in children," says Jennifer Furin, an infectious diseases clinician at Harvard Medical School who has been working with TB in developing nations for more than two decades.
So far the South African program has enrolled more than 300 families and provided preventive treatment to 200 children, none of whom developed the disease. The project can serve as an example, Furin says. "We have to focus on prevention in households if we want to make a dent in the TB epidemic."
TB behind Bars
Prisoners are another neglected group in the TB pandemic, and they often face an unintended sentence. Conditions such as overcrowding, poor ventilation and poor nutrition make them susceptible to the disease. And because most convicts enter prison with prior risk factors such as malnutrition and substance use, they are even more vulnerable.
Last August, Eduardo da Silva, a 22-year-old inmate in a prison in the state of Mato Grosso do Sul in southwestern Brazil, had the misfortune to face all these conditions at once. Locked behind a thick steel door, a tiny hole his only window, da Silva was wracked with fever, cough, chest pain and night sweats. Other convicts forced him to sleep in a corner on the cold floor, thinking he had COVID. Isolating was impossible because da Silva shared a cell twice the size of a king-size bed with more than 50 people. "I couldn't do anything but lie down," da Silva recalls, but space in the cell was so tight that people often slept in a sitting position or on top of one another.

He had no energy to walk or eat, and in two months his weight plummeted to 89 pounds. It was TB, not COVID.
It has become a common story in South America. While TB has declined across the world, here it has surged along with incarceration. The incarcerated population grew by 200 percent in the past two decades. Among that group, TB cases more than doubled from 2011 to 2017, according to a Lancet study. Brazil accounts for almost half of that increase. Those entering prison in Brazil have roughly average infection rates, but their risk increases 25 percent each year of incarceration, according to a study co-authored by Julio Croda, an epidemiologist at the Federal University of Mato Grosso do Sul. "Prisons are TB amplifiers," Croda says. "But unfortunately, most people in society don't care about what happens in prisons."
They may not care, but prison walls are not strong enough to keep TB inside. The disease spreads among inmates, visitors and workers alike. To trace the path of infection, Croda and his colleagues compared the genomes of TB bacteria sampled from prisoners and recently released convicts. In Mato Grosso do Sul, they identified at least 18 chains of contagion by which prisoners and ex-convicts transmitted TB to others. In one sample of 320 cases of people never incarcerated, half were directly connected to prisoners. Because TB can remain dormant, researchers have found inmates may become ill and infectious up to seven years after release.
Croda and his colleagues are developing a strategy to stop this spread, conducting mass screenings in three major Brazilian penitentiaries in Mato Grosso do Sul. Since 2017 they have tested more than 7,000 inmates for TB every nine months using the standard sputum test plus artificial-intelligence software that assesses chest x-rays.
When da Silva was diagnosed with advanced TB, he was scared. His father had had TB in prison and was never properly treated, so he did not realize the disease was curable. After counseling and treatment, his confidence grew. "I felt the health team cared about me, and they told me I would be cured," da Silva says. "So I took the medicines."
TB spreads quickly in prisons, but it also can be better controlled there because prison staff ensure treatment adherence. "Everyone in the cell helps each other to keep the treatment going," says Andrea Santos, a nurse with the project. The intervention cut TB cases by half in one prison in Mato Grosso do Sul. Predictive models designed by Croda and his collaborators suggest that mass screening in prisons can reduce TB prevalence in surrounding communities by nearly 20 percent.
After six months of treatment, da Silva is cured. He is back to his normal weight and says he feels good. But he is an exception. Mass-screening programs for TB in prisons are rare because there is a general failure to recognize the role of prisons in the disease. The WHO does not keep any official record of TB cases among prisoners or list them as a risk group. "We won't reduce TB incidence, especially in South America, if we don't address this population," Croda says.
Fighting a Social Disease
The COVID pandemic amplified an important lesson in public health: conquering a disease requires multiple combined efforts. "We learned with COVID that masks were good, but not enough. Isolation was good, but not enough. Vaccines were good, but also not enough," Pai says. "Now is the time to do the same with TB."
A comprehensive approach to TB requires investment in screening, preventive therapy and better drugs but most of all in fighting poverty. Universal health care and increased income correlate directly with a drop in TB rates. To make real progress, Pai notes, governments and public health organizations must tackle social aspects of the disease, such as stigma, crowded living conditions, malnutrition and the economic burden of treatment. "If we focus on only the biomedical aspects of TB, we can make an improvement, but we will never control the epidemic," he adds. "There is no way to really solve TB without tackling inequality."
This article is part of "Innovations In: Health Equity," an editorially independent special report that was produced with financial support from Takeda Pharmaceuticals.
This article was originally published with the title "The Oldest Pandemic" in Scientific American 326, 6, - (June 2022)

Comments
Post a Comment